Pectus Carinatum
Pectus Carinatum (PC) is a thoracic deformity in which an abnormal costal cartilage growth produces an outward anterior chest wall protrusion described as “pigeon chest”.
PC is considered the second-most common cause of thoracic malformation after pectus excavatum (PE), with a reported incidence ranging from a fifth of PE in some centres, to arrive to an equal incidence in others. It is more prevalent in males with a ratio of 3-4 to 1.
PC is often noted in childhood with progression during adolescence.
PC malformations could be classified according to the shape of the protuberance in symmetric (photo 1) and asymmetric defect (photo 2) and in chondrogladiolar or chondromanubrial defect depending if the site of sternal angulation is located at the body of the sternum or at the manubrium. The chondrogladiolar is the more common one.
PC can be also a secondary malformation, occurring after sternotomies for cardiac surgery or following surgical PE repair.
Diagnosis is made by physical examination and the elasticity of the sternum and related deformed costal cartilages can always be assessed by manual compression or by means of pressure-measuring devices.


Photo 1: Symmetric PC Photo 2: Asymmetric Pcù
Author
Antonio Messineo, M.D.
References
Mantinez-Ferro et al. Seminar in Ped. Surgery. 2008
De Beer et al. Ann. Thorac. Surgery. 2017
Fraser et al. Ann. Thorac. Surgery. 2020
Quality of Life
Pectus carinatum often results in a reduced quality of life (QoL) due to a disturbed body image and lower self-esteem. Several studies have shown a significant reduction of QoL. After correction of the deformity, pectus patients had a significant improvement of QoL.
Author
Caroline Fortmann, M.D.
References
Paulson et al. J Pediatr Surg. 2019
Bostanci et al. J Pediatr Surg. 2013
Knudsen et al. J Pediatr Surg. 2015
Bracing
Over last years, bracing for pectus carinatum has gained significant popularity, and this has been corroborated by the increasing number of publications on bracing versus surgery. However, this form of therapy was not new as the first reports were published almost three decades ago. Most recent reviews, endorse bracing as first line treatment for pectus carinatum and it has demonstrated to be effective to treat both, symmetric and asymmetric cases.
A wide range of commercially available braces are available, some of them include pressure measuring capabilities although local orthotics departments are also capable of creating their own pectus carinatum braces.
It is highly likely that a bracing program is more important than the brace itself and prescribing a brace alone is unlikely to result in success. Continued follow-up during treatment, with frequent adjustments, assessment of patient progress, and maintenance of patient motivation, is essential.

Fig 1. Symmetric Pectus Carinatum: Results after 9 months of treatment of a 13-year-old patient with severe symmetric pectus carinatum using a Dynamic Compression System. Pressure of initial correction (PIC) 6,5 PSI
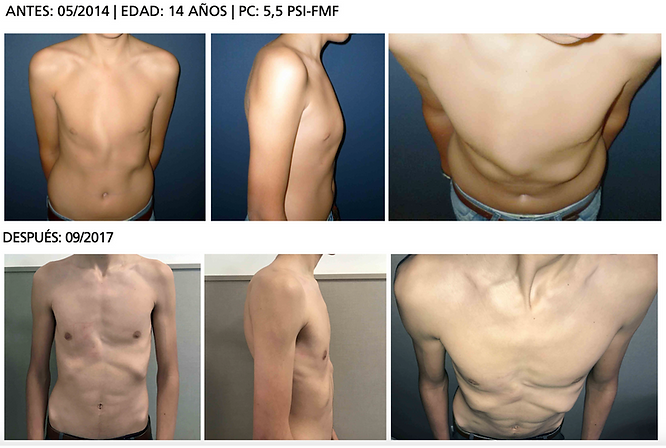
Fig 2. Asymmetric Pectus Carinatum: Results after one year of treatment with late follow-up pictures (2.5 years) of a 14-year-old patient with severe asymmetric pectus carinatum using a Dynamic Compression System. Pressure of initial correction (PIC) 5,5 PSI
Author
Marcelo Martinez-Ferro, M.D.
References
Haje et al. J Pediatr Orthop 1992
Martinez-Ferro et al. Semin Pediatr Surg. 2008
Emil et al. Eur J Pediatr Surg. 2018
de Beer et al. Semin Pediatr Surg. 2018
Minimally-invasive repair of pectus carinatum
The criteria for selecting patients to be eligible for minimally-invasive repair of pectus carinatum (MIRPC) are mainly based on the elasticity of the thoracic wall. The ideal timeframe for the operation is the period of rapid body growth. Both symmetric and asymmetric clinical forms can be corrected using the MIRPC method.
In this technique, the sternochondral region is compressed by implanting a metal bar subcutaneously in the presternal region and securing it bilaterally to the posterolateral portion of the costal arches. The implant consists of a compression strut and fixation plates. The two fixation plates, which are fixed to the compression strut with screws, are rectangular in shape and have holes at the ends that allow the plates to be attached to the ribs by means of steel wire suture. Correction of the chest contour and simultaneous lateral expansion of the depressed costochondral arches are achieved by compressing the protruding anterior region of the chest wall. The strut remains implanted for 2 – 3 years.
Bar adherence to patient skin has been a frequent complication. It is highly recommended to concentrate in modeling the implant bar to match it as much as possible with the chest shape, to achieve a minimal contact with the skin.
Fig. 1: Model of the implanted bar and fixation plates on the ribcage
Fig 2a – 2c: Symmetric Pectus Carinatum: Results of 3 patients who underwent MIRPC (before and after correction)
Fig 3a & 3b: Asymmetric Pectus Carinatum: Results of 2 patients who underwent MIRPC (before and after correction)
Author: Horacio Abramson, MD
References
Abramson H. Arch Bronconeumol 2005
Abramson et al. J Pediatr Surg 2009
Geraedts et al. J Pediatr Surg 2022
Katrancioglu et al. Asian J Surg 2018











The Sandwich Technique
The sandwich technique is based on the press-molding to evenly remodel the chest wall, by applying counter-forces to compress the carinated portion and internal support to prevent the surrounding areas from being aggravated and ultimately the entire anterior chest wall to achieve an anatomically normal chest wall. The external bar applies pressure to compress the carinatum, while the internal bars provide support to the chest wall from underneath, resulting in a reshaped and flattened chest wall.
The primary repair target is marked on the top of the carinatum, with secondary targets on the depressed portions of the chest wall. First, the internal bars that conform the chest wall morphology are introduced using pectoscopic dissection. The internal bars are to elevate the depressed portion of the chest wall and support it against the upcoming external bar compression. The external bar, with a flattened segment for more compression on the carinated part, is placed subcutaneously onto the apex of the chest wall protrusion to press down on the carinatum. Finally, the external and internal bars are connected to the bridge plate while compressing the carinatum using a table-mounted compressor finally to form a fortress cage to squeeze (press-mold) the chest wall.
Parallel bar sandwiching: two internal bars in a parallel pattern and the external bar between them.
Cross-bar sandwiching: placing two internal bars in a crossed pattern and the external bar between them. This technique is used to cover the lower bilateral costal depressions.
Author: Hyung Joo Park, MD
References
Park et al. Ann Cardiothorac Surg 2016




Modified Ravitch Procedure
In the case of chondrogladiolar PC, the general concept of the modified Ravitch operation also applies. Once a subperidondrial resection of all deformed cartilage has been obtained, and the sternum has been corrected at the same level as the insertions of the intercostal muscles, one or two osteotomies of the anterior table can be performed if necessary, allowing the sternum to be fractured and displaced posteriorly, almost exactly as we explained for PE.
In cases of a chondromanubrial deformity (see also “Currarino-Silverman-Syndrome” in the subgroup “others”), a titanium plate is also recommended to repair the transverse osteotomy of the sternum, with which it is possible to obtain adequate correction and a better position of the chest wall (Figure 1a & b). In most cases the resection can be a larger triangle than a simple transverse osteotomy


Figure 1a & b: System of parallel plates to repair the transverse osteotomy of the sternum. This allows the young patient to have a sternotomy, if it is ever necessary.
To finish the procedure, the pectoralis major muscles have to be brought together, which requires a submuscular suction drainage for a few hours, and closure of the subcutaneous tissue and skin with running sutures.
Author
José Ribas Milanez de Campos, M.D.
References
Ravitch. J Thorac Surg. 1952
Sulamaa et al. Acta Chir Scand. 1959
Haller et al. Ann Surg. 1976
Mao et al. J Pediatr Surg. 2017
Shamberger et al. J Pediatr Surg. 1988
